December 06, 2021
By Patricia DiJoseph, Ph.D.
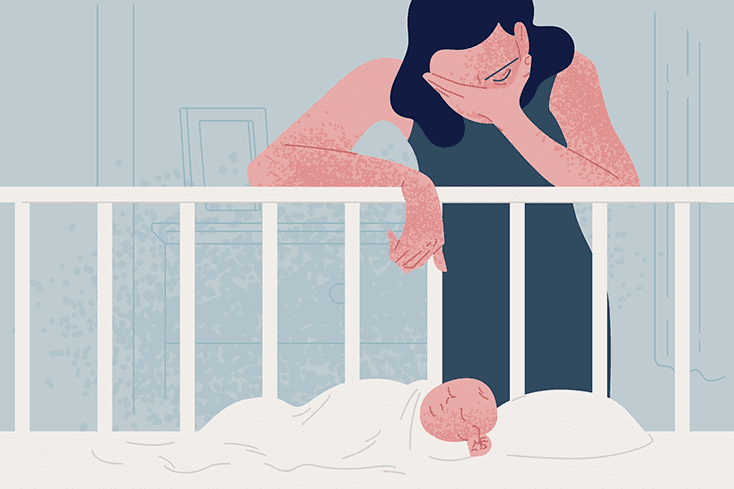
Looking back, I had all the classic symptoms — and they were severe.
I believed someone had to be in the back seat with my son Thomas in the car; otherwise, he’d die. I believed I had to stay awake all night while I was watching him, otherwise, he’d die in his sleep. I feared “the agency” was going to come at any moment and take him back and say he wasn’t mine. These fears were all so real to me — never did I think, “I have an illness, and with help I can get better.”
The thoughts got worse, now telling me in detail to commit the gravest sin. I hated those thoughts, the thoughts of hurting my baby, and I didn’t want to listen to them.
Day and night, I would be on guard in case they came. When they did come, I would use all my willpower to bury them. It was mentally and emotionally exhausting. I was terrified because I thought, “What if they win and my strength fails me?” or “What if I actually act on them?”
When the thoughts kept coming — and their frequency increased — somewhere deep down, my intellect kicked in, and I knew I needed to see a psychiatrist.
Seeking Help
I still had no idea that I was experiencing postpartum OCD and depression, but I did know the terrible thoughts meant my brain chemistry was off.
When I talked to a doctor, he said I’d get better the fastest if I went to an inpatient mental health facility. I agreed, as I just wanted to get better. He described me as homicidal to the facility while trying to secure me a spot. So, that is how I began to see myself. Even after a week in the facility (and over two months of partial inpatient and outpatient therapy), I still believed I was a threat to my baby. I was told I couldn’t be alone with him. No one told me differently. The fear of hurting my baby overtook my whole life. I was no longer me; I was no longer confident, I had no joy, I had no self-love.
We all have blessings in our life. Four months after being told I was homicidal, we moved to a different state due to my husband’s new job. I got a new psychologist and psychiatrist who specialized in maternal medicine and therapy. They recognized that my intrusive thoughts were, in fact, symptoms of OCD. They assured me that I wouldn’t act on my thoughts. Their assurance immediately lifted the largest weight from my shoulders. I did not have to fear myself anymore and always be on guard.
My therapist taught me how to recognize and ground myself when I had these alarming thoughts. With the professional help I needed, I came to accept that no grave harm would come to my baby, either from myself or elsewhere, so the intrusive thoughts held little weight and no longer effected my day-to-day living.
What I Learned
I learned that the people who truly care will still love you. My relationship with my husband is better than it’s ever been (learning emotional intelligence and communication skills in therapy has been great for our marriage). I’m still very close with my family. I know they always want me to do well. I also am fortunate to have the best girlfriends who I still love getting together and having open, honest conversations (I even learned that some also experience mental illness).
I learned sympathy for those with mental illness. I understood intimately how some people might not even know that there is a path to recovery — that we just need the right help to get there. Sometimes, we need medicine. Sometimes, we need to train ourselves to think, process and react in new ways.
I learned that we need more experienced mental health practitioners and psychiatrists. We need caregivers to be familiar with all the proper signs, diagnoses and treatments for mental health.
I learned we need dedicated support for families who are drained from taking care of their loved ones with mental illness. We all need to be checked on; not just “how are you” but “I’m concerned. Please take this mental health survey and let’s see if there are any warning signs.”
I learned that mental health should be prioritized early in life (at school and at home). We go to the dentist twice a year to have shiny white teeth. Can we approach mental health the same way? Imagine if everyone was taught that it’s important to go see a professional when you are struggling.
I learned I am strong. I am as strong as they come. I opened up about the awful thoughts in my head as I knew something needed to change. I never gave up. I was at a very low point during the period that I thought I was homicidal, but I just kept trudging through. I’m a more joyful person now than I was before this experience.
I’m very pleased with all my progress. I still see a therapist weekly and a psychiatrist monthly and take prescribed medications regularly. I hold a professional job in research and development of engineering technologies and, importantly, I love being a mommy.
Dr. Patricia DiJoseph lives in Virginia. Hew newest joy is playing, reading and cuddling with her two-year-old and getting to see him explore the world with fresh eyes. Patricia holds a Ph.D. in Transportation and has learned that there is something harder than writing a doctoral dissertation — navigating mental illness.
Submit To The NAMI Blog
We’re always accepting submissions to the NAMI Blog! We feature the latest research, stories of recovery, ways to end stigma and strategies for living well with mental illness. Most importantly: We feature your voices.
LEARN MORE