What to Look For and When to Act
While each mental health condition is unique, they all impact emotions, thoughts and behavior. Here are some things to consider in deciding to intervene.


Find local support
Connect with a NAMI chapter near you
Select your state to find a local NAMI affiliate. The page will redirect to the affiliate's page when a state is selected.

In need of help or support?
If you are struggling with your mental health, there are a variety of ways to connect with NAMI. Get immediate support by calling, texting or emailing.
Disruptions in Daily Interactions and Relationships
Everyone experiences a “bad day” from time to time, but when your child seems to be having difficulty with routine daily tasks, it’s important to take notice. This can look like difficulty participating in regular social activities (with family, friends, adults), academics, or play/activities.
It can also look like a change in personality. For example, if your child is typically socially interactive, but begins to withdraw and has no interest in others, this could be an indicator of an underlying mental health issue. If you notice these types of changes, and they last for more than a few weeks, it may be time to reach out to a professional for support.
Excessive Anxiety
Anxiety is a typical reaction to situations that we perceive as potentially dangerous or where performance has a possible negative effect (like failing a test or losing a game). But when the amount of anxiety or stress is out of proportion to the reality of the risk, you should pay attention to these reactions. It’s time to consider intervening if your child:
- Worries about almost everything to the point of withdrawal or has difficulty functioning
- Is fearful of certain places (such as school) or going to new places
- Experiences sudden bursts of intense fear, impending doom, or physical symptoms such as rapid heart rate, hyperventilation, dizziness, or nausea
- Believes they must repeat certain thoughts (obsessions) or behaviors (compulsions) to prevent something bad from happening
Depression
It’s normal for everyone, including children, to feel “down” from time to time, especially during challenging life situations. However, if your child is experiencing ongoing difficulties with any of the following symptoms, it might be a good idea to seek support:
- Disturbances in mood (usually irritability in children, compared to deep sadness in adults)
- Impaired sleep (typically too much sleep, but some may have trouble falling or staying asleep)
- Decreased energy
- Decreased self-esteem
- Difficulty concentrating
- Change in appetite (typically excessive appetite or, more rarely, reduced appetite)
- Seems agitated or, conversely, “slowed down”
- Expresses thoughts of hurting themselves or thoughts of suicide
Substance Use
Be on the lookout for changes in behavior that may be due to using substances, including alcohol, marijuana products, psychedelic drugs, prescription medications, and others. Substance use may also extend to misuse of over-the-counter drugs or medications prescribed to other people (typically friends or family).
If your child is using substances, you may observe a decline in school or sports performance, decreased engagement with family or friends, sleep problems, and sluggish or agitated behavior. Treatment for substance use can be very helpful.
Changes in School Performance
Some children have challenges with standard academic work. However, if your child typically performs well and begins having difficulties, there may be an underlying mental health condition to blame. If academic challenges persist, it may be helpful to consult with a clinician.
Acute or Prolonged Stress
A child witnessing violence or experiencing abuse/neglect at home will most likely experience acute or prolonged stress. Post-traumatic stress disorder (PTSD) can be the result of these traumatic experiences and may include symptoms like:
- Disturbances in memory issues, such as flashbacks
- Recurrent thoughts of the trauma
- Emotional numbing, such as avoiding social and emotional contact with others
- The emergence of a hyper-state of arousal, like they might panic at any time
It is important for anyone experiencing trauma to be able to process, or work through, those experiences. Meeting with a professional can be helpful.
Difficulties Adjusting
Children, like all of us, respond to difficult situations in their own way. Those reactions can include increased anxiety, depression, or a mixture of emotional reactions. Common situations that contribute to adjustment difficulties include grief and loss (such as death of a loved one or divorce), changes in a parent’s employment, military deployment of a parent, domestic violence, bullying, or harassment. If your child seems to be struggling after experiencing a certain event or situation, it can be helpful to talk with a professional about what you are observing.
What To Do
It can be extremely difficult when your child experiences mental health symptoms, but there is hope. Below are some actions you can take to help your child.

Have Frequent Conversations About Mental Health
Even if your child isn’t experiencing any difficulties, it’s always helpful to engage in frequent emotional “check ins” starting early in life. If your child sees this as a routine part of family life, they will likely feel more comfortable coming to you when they experience challenges. Additionally, if you notice something seems off with your child and ask them about it, they may be more receptive to sharing with you.
NAMI resources for starting conversations about mental health:

Language Matters
Tips for talking about mental health and suicide.

10 Questions on a Tuesday
Ask any of these questions to develop practical strategies with your child on how to best support their mental health.

A Week of Wellness
Use this wellness calendar daily to incorporate different activities into your everyday.
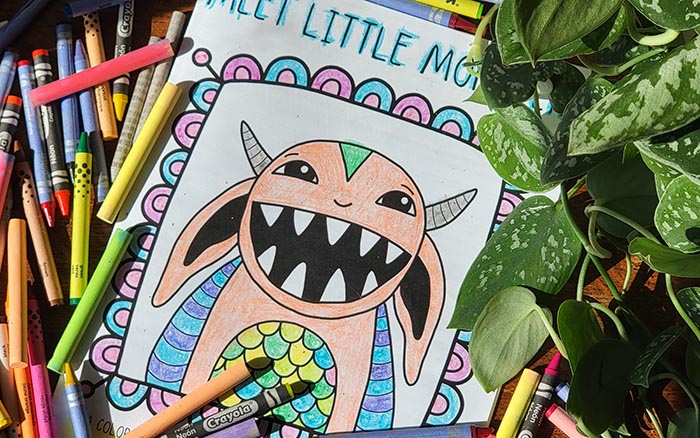
Meet Little Monster
A coloring and activity book that helps children express and explore their feelings in a fun, creative, and empowering way.
Listen and Validate Their Feelings
While you may not understand what is upsetting your child, making your home a place where you child can share openly without fear can suggest you’re eager to hear about their life in a supportive, non-judgmental way. This paves the way for your child to see you as an ally, not as a judge.

How to be a Trusted Adult
A trusted adult is someone who
is not a parent/caregiver but is
part of the child’s safe natural
network through family and
other institutions.
Get Feedback From Others
While your observations and perceptions may be accurate, consider talking with siblings, other family members, teachers, coaches, clergy — or anyone in your community who knows your child — to see if they have noticed changes in their behavior. Hearing others’ perspectives may help to determine how severe the problem is and to decide what the next steps should be.
Get a Professional Opinion
If you are concerned, there is no harm in talking to your pediatrician or other health care professional about whether they think your child could benefit from seeing a mental health professional. They can also be helpful in providing resources or referrals in your community.

We want to hear your story
Tell us how mental illness has affected your life. What has been challenging? What has been helpful to you?
Additional Resources

NAMI Basics
A free education program for parents, caregivers, and other family who provide care for youth (ages 22 and younger) who are experiencing mental health symptoms.

NAMI TraumaInSight
For youth-serving professionals who want to support young people who are struggling with trauma and challenging emotions.